Which of the Following Is Prohibited by Medicare
Dino proceeded to verify the consumers Medicare eligibility describe the costs and benefit coverage of the plan and explained that he could not accept an enrollment application until October 15. Speech-language pathology services durable medical equipment orthotics and prosthetics are included in.
Medicare Rates As A Benchmark Too Much Too Little Or Just Right Altarum Healthcare Value Hub
Benefits must automatically change to coincide with changes in medicare deductibles and copayments.
. Prohibited abbreviations in the medication orders from one of the sites were analyzed to determine the designation of prescribing staff who used the abbreviations. C People of any age who have been entitled to disability benefits for 24 months D People suffering from liver cancer. Rueppel is the Digital Content Producer at Ritter Insurance Marketing.
Which of the following statements about medicare supplement plans is false. The Marketing guidelines reflect CMS interpretation of the marketing requirements and related provisions of the Medicare Advantage and Medicare Prescription Drug Benefit rules Chapter 42 of the Code of Federal Regulations Parts 422 and 423. Medicare Marketing Guidelines.
Prior to Ritter Sarah worked in radio and television after graduating from Kutztown Universitys Professional Writing program. Which of the following statements would be prohibited. Mandatory refund on any payments previously received.
Which of the following are NOT eligible for Medicare coverage. Medicare Claims Processing Manual. Losses resulting from sickness may not be treated differently than losses resulting from accidents.
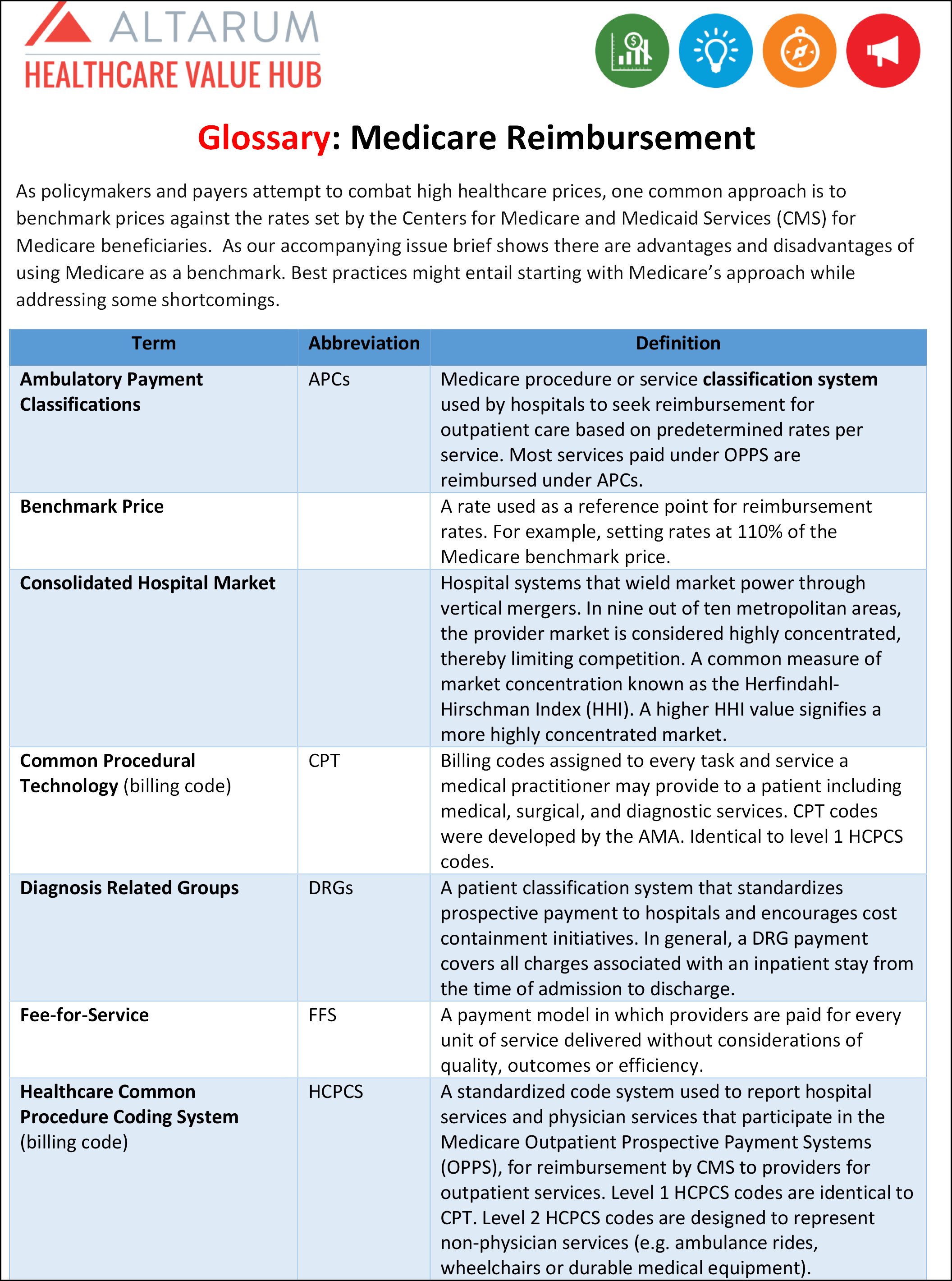
Dino an agent received a phone call on September 29 from a consumer interested in Medicare Advantage plans for the new plan year. For Medicare Advantage Plans. Upon admission Prospective Payment System PPS hospitals and acute care.
Medicare Online Enrollment Center OEC. However individuals who already have Plans C and F will be able to keep their current versions of the plans and individuals eligible for Medicare prior to January 1 2020 can. Chapter 2 - Admission and Registration Requirements.
The Stark II law introduced by Rep. Therefore Plans C and F will no longer be an option for newly eligible individuals starting January 1 2020. Which of the following statements if any is true regarding the Stark Law.
Part D plans must enroll any eligible beneficiary who applies regardless of health status except in limited circumstances. Hospital coinsurance payments Medicare covers the first 60 days in full after the deductible has been met. 1 The patient must first be admitted to an acute care hospital for a minimum of 3 days 2 The patient must have a documented medical need for skilled care and services 3 The patient must meet verified.
Medicare payment 80 percent of the MPFS allowed amount less 5 percent 342 Medicare write-off not to be paid by Medicare or the beneficiary 15837 Calculate the following amounts for a nurse practitioner who bills Medicare. Which of the following statements about Medicare is most correct. Prohibited from balance billing patients Which one of the following types of care is not covered by Medicare Part A.
Pete Stark D-CA designates ten categories of Medicare and Medicaid health services for which self-referral is prohibited. Denial of payment -- payment by Medicare or Medicaid for designated health services that are furnished in violation of the Stark law is also denied. Medicare Secondary Payer MSP is the term generally used when the Medicare program does not have primary payment responsibility - that is when another entity has the responsibility for paying before Medicare.
Prohibited on the paper enrollment mechanism eg impermissible health screening. Specifically for individuals newly eligible to Medicare the Part B deductible cannot be covered. Question 22 1 point Which of the following is NOT a condition that must be met in order for Medicare to cover a patients stay in a skilled nursing facility.
This preview shows page 21 - 24 out of 41 pages. Which of the following best describes the situation of a provider who agrees to accept assignment for Medicare services. Hospital deductible per spell of illness.
Dos and Donts of Medicare Compliance. The Guidelines are for use by Medicare Advantage Plans MAs Medicare. 1 Medicare Advantage Prescription Drug Plans Prescription Drug Plans EmployerUnion-Sponsored Group Health Plans Medicare -Medicaid Plans and Section 1876 Cost Plans.
Exclusion from the Medicare and Medicaid programs iv. Statements a b and c. Potential penalties under Stark Law i.
When completing an enrollment application in LEAN why is an agent prohibited from entering their own email address in a field available for the consumers email address. The consumermember would not receive plan related correspondence intended. The following is a general description of requirements and prohibited activities that apply to admission for inpatient services or registration for other healthcare services.
When Medicare began in 1966 it was the primary payer for all claims except for those covered by Workers Compensation Federal Black Lung benefits. Medicare beneficiaries pay neither deductibles nor copayments for healthcare services received. Civil money penalties of up to 15000 per prohibited referral iii.
Medicare is administered by the Centers for Medicare and Medicaid Services CMS. The plan sponsor is approved for. The cost plan may not request or collect financial information eg a credit card or bank account number or market or enroll beneficiaries in other lines of businessproducts as part of the online enrollment process.
These benefits are Medicare-approved O C. Table of Contents Issued. 2021 United HealthCare - Ethics and Compliance.
These sanctions are imposed on the organization or DHS entity that receives the prohibited referral and that bills Medicare for the service ie the physician-owned medical practice a hospital or another service provider. She began writing for Ritter and the Agent Survival Guide blog in 2016 and now hosts our podcast. This plan is number one O B.
Which of the following statements about Medicare Part D are correct. The following is a partial list of gaps in coverage that are not reimbursed by Medicare. In terms of events which of the following is true.
Days 61 to 90 require a copayment and days 91 to 150 the lifetime reserve days a higher. Medicare Marketing Guidelines. A People age 65 and older who are eligible for Social Security B People age 65 and older not eligible for Social Security but willing to pay a monthly premium.
The following categories of prescribers were audited. According to the Medicare Communications and Marketing regulations CMS prohibits the distribution of materials that are misleading inaccurate or otherwise make misrepresentations.

Via Twitter Learn More About This Project By Clicking Through Medicare Outreach Projects Advocacy
Medicare Rates As A Benchmark Too Much Too Little Or Just Right Altarum Healthcare Value Hub
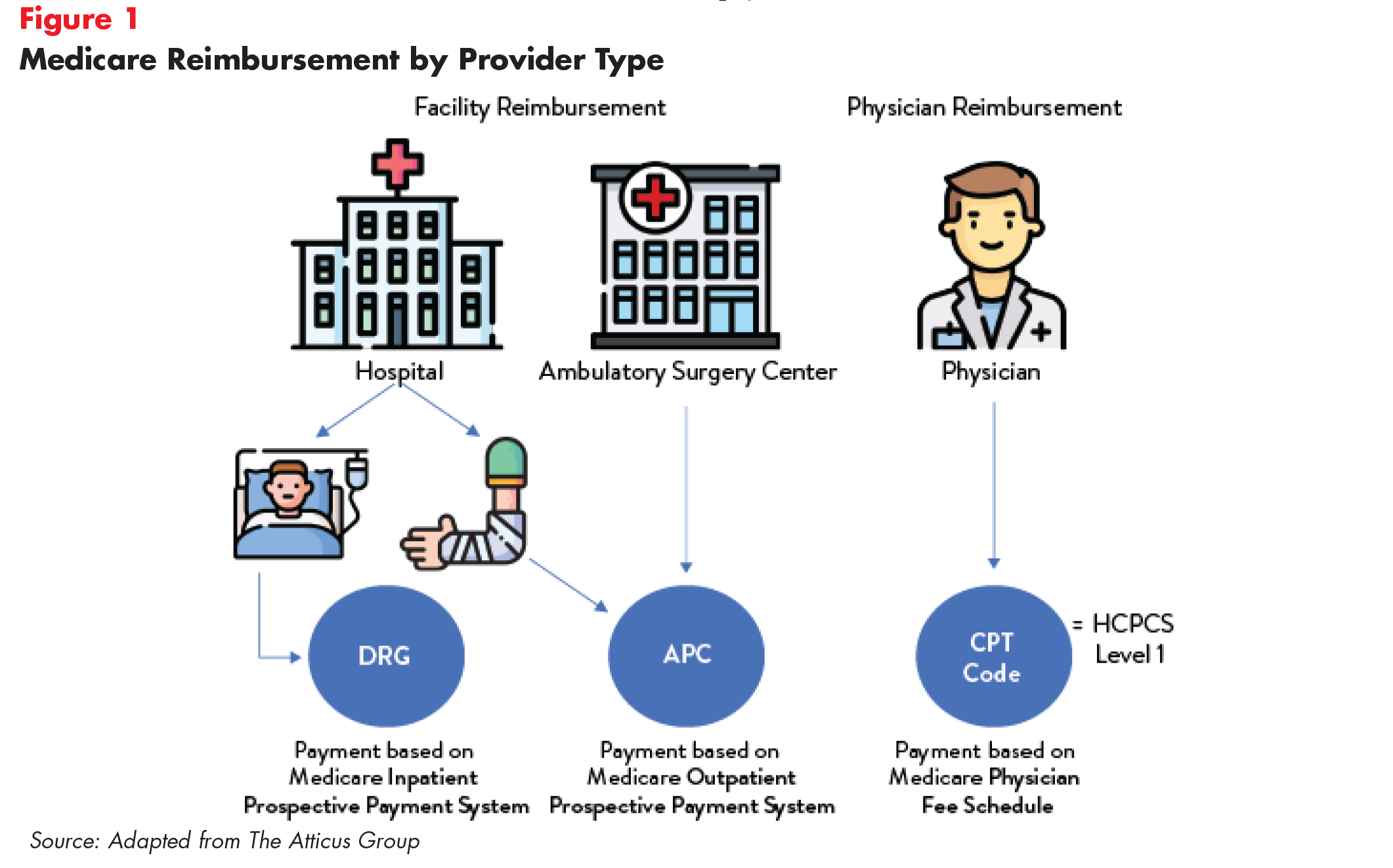
Medigap Enrollment And Consumer Protections Vary Across States Kff
Comments
Post a Comment